Understanding Cervical Cancer | Early Signs, Risk Factors & Prevention
文章作者: Dr Ooi Poh Siang, Family Medicine Specialist
09 January 2026
Cervical Cancer: Preventable, Treatable, and Beatable
Every January, we observe Cervical Cancer Awareness Month. Represented by the teal and white ribbon, this month is a vital reminder that cervical cancer is one of the most preventable forms of cancer. Through vaccination and regular screening, we have the power to protect ourselves and our loved ones.

The Current Situation in Malaysia
According to the latest National Cancer Registry Report (2017–2021), cervical cancer is the sixth most common cancer among women in Malaysia.

There is good news: the incidence rate is steadily decreasing. It dropped from 7.6 per 100,000 women (2007–2011), 6.2 per 100,000 women (2012–2016) to 6.0 per 100,000 women (2017–2021). This progress is thanks to our national vaccination and screening programs. However, a concerning 47.1% of cases are still diagnosed at late stages (Stages 3 & 4), which highlights the urgent need for earlier detection.
Knowing the Signs and Risks
Most women with early-stage cervical cancer have no symptoms at all. This is why screening is so important.
However, you should consult a doctor immediately if you experience:
- Bleeding after menopause.
- Bleeding after sexual intercourse.
- Unusual vaginal discharge.
- Persistent abdominal pain.
The Human Papillomavirus (HPV) is the primary cause of cervical cancer. Other factors that can increase your risk include:
- Having more than three sexual partners.
- Starting sexual activity at a young age (under 17).
- Long-term use of oral contraceptives (over 10 years).
- Giving birth to your first child before age 17.
- Having many children (7 or more).
- Smoking.
- Lower socioeconomic status.
Early Detection: Pap Smears and HPV Tests
Because cervical cancer develops slowly, catching it early makes it highly treatable. Cervical cancer is unique because it is almost entirely caused by HPV. Understanding how this virus works is the key to why we can eliminate this cancer. There are over 100 types of HPV. While many are harmless, about 15 "high-risk" types are known to cause cancer.
Most people will get HPV at some point in their lives, and the body usually clears it on its own. However, in about 4% to 10% of women, the infection doesn't go away. This is called a persistent infection. It typically takes 10 to 15 years for a persistent HPV infection to turn healthy cells into cancer. This "slow-motion" process is exactly why regular screening (Pap smears and HPV tests) is so effective—it gives us a huge window of time to catch and treat the problem before it ever becomes cancer.
In Malaysia, roughly 7% of healthy women carry the HPV virus. Without screening, these women are at a higher risk of developing cervical cancer later in life.
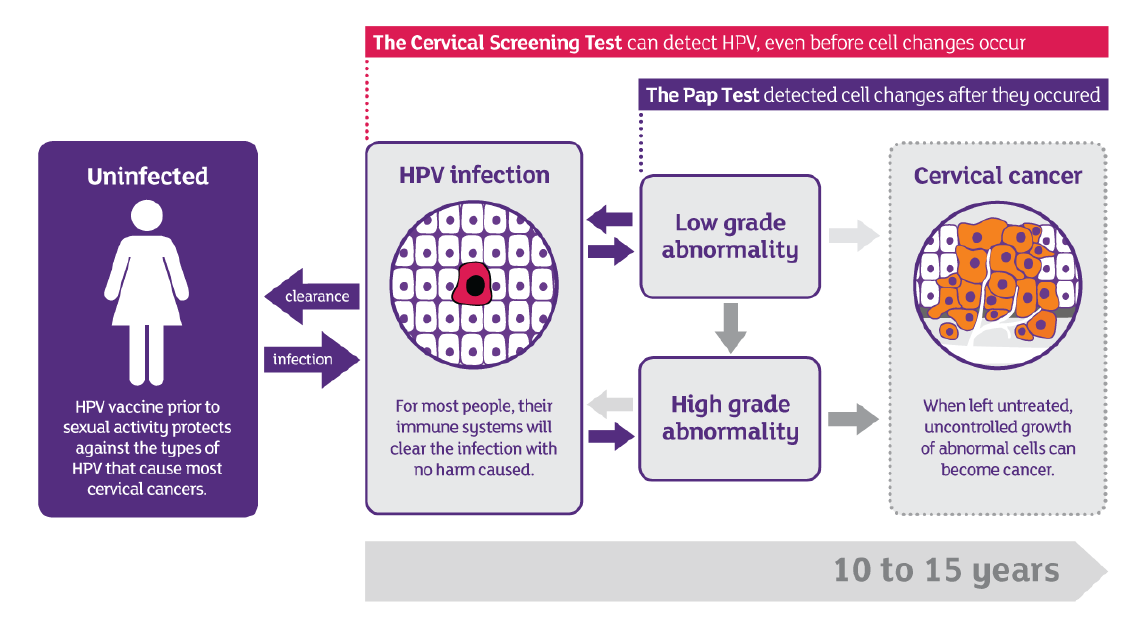
*Picture from Guidelines For Cervical Cancer Screening In Malaysia 2023
Who Should Get Screened?
- Cervical cancer screening is offered to all sexually active women.
- Women under 30: Recommended for a Pap smear.
- Women aged 30 – 65: Pap smear and / or HPV test.
- Women over 65: If you have never been screened, an HPV test is recommended.
How Often Should Screening Be Done?
- For Pap Smears: Once a year for two years. If both are normal, you only need to go every 3 years.
- For HPV Tests: If the result is negative, you only need to be re-tested every 5 years.
Preparing For Your Cervical Cancer Screening:
- Avoid taking cervical cancer screening during normal menstruation. If abnormal or prolonged menses, refer to doctor.
- Avoid sexual intercourse 48 hours prior to the procedure.
- Do not douche or insert any form of medication or tampons (vaginal creams, foams, films, or jellies or spermicides) into the vagina 48 hours prior to the procedure.
- Any cervical lesion seen should be referred to O&G specialist.
- Can be performed after 6 weeks post-delivery.
Even though screening services are widely available in Malaysia, the number of women coming forward for testing remains low, with participation rates between only 23% and 26%. This coverage dropped by as much as 50% following the COVID-19 pandemic. I strongly encourage everyone who is eligible to come forward and get tested.
Protection through Vaccination

Since 2010, Malaysia has provided HPV vaccinations to 13-year-old schoolgirls. This protects them before they are ever exposed to the virus. Research shows this can prevent up to 89% of cervical cancer cases.
Missed your school vaccination? It’s not too late. Adults up to age 45 can still get vaccinated. For those aged 15 and older, a 3-dose schedule (at 0, 1–2, and 6 months) is required.
A Future Without Cervical Cancer
We are moving toward a world where this disease no longer claims lives. Australia is set to lead the world as the first nation to eliminate cervical cancer, with a target date of 2035. A major milestone was reached in 2021 when, for the first time since 1982, no new cases were diagnosed in women under the age of 25. Additionally, survival rates for the disease continue to rise. Closer to home, Sarawak has set an ambitious goal to be free of cervical cancer by 2030.
We have the tools—vaccines and screenings—to make this a reality. If you are eligible, please come forward for your check-up. It is a simple step that can save your life.
References
- Guidelines For Cervical Cancer Screening In Malaysia 2023
- Clinical Practice Guidelines, Management of Cervical Cancer Second Edition 2015
- Summary of Malaysian National Cancer Registry Report (2017-2021)
- Australia on track to eliminate cervical cancer by 2035, Australian Government Department of Health, Disability and Ageing, posted on 19 Nov 2025
- Sarawak Aims To Be Free Of Cervical Cancer By 2030, UKAS, posted on 03 Aug 2024